Palliative care nurses: Bedside angels to the dying and their families
This series of interviews commemorates Singapore Nurses' Day on August 1, 2020. Salt&Light salutes all nurses for their dedication and care!
Tan Huey Ying & Anna Cheang // July 30, 2020, 12:36 am

Sister Eliada (third from left) with her team of palliative care nurses at Assisi Hospice. For Nurses' Day 2020, Assisi has launched an “I Care For Assisi Nurses (I C.A.N)” campaign, where members of the public can read the stories of our nurses and write a note of appreciation to show their support for them: www.icareforassisinurses.sg. Photo courtesy of Assisi Hospice.
When Ng Xinhui turned 21, her 30-year-old brother was diagnosed with end-stage colon cancer. Three years later, he passed away.
In 2019, Ng turned 33 – the same age that her brother was when he died.
It was the final push she needed to enter palliative care after 13 years as a ward nurse in Singapore General Hospital’s haematology department, caring for patients with blood disorders.
Palliative care has always been particularly meaningful to Ng. She knows too well the journey that awaits a patient and the loved ones as death approaches.
Against the grain
Palliative medicine, which includes end-of-life care, focuses on improving the quality of life for patients with life-threatening illnesses through the prevention and relief of the illness-induced suffering.
It is a relatively new field developed in the late 1940s in Britain. The first palliative care service in Singapore was started only 35 years ago in a home for the aged where 16 beds were set aside for terminally ill patients.
The word, “palliative”, throws many people off, Ng said. “There is a stigma associated with the idea it, a resigned waiting for death to come.”
But during her student attachment to palliative care, Ng recalled the impression it had made on her.
“The nurses treated the patient as a person – it was as simple as that.”
In medicine, it is all too easy to treat patients as medical problems to be treated and “sorted out”, Ng explained. What had attracted her then, was the way the nurses respected the patient and the family, taking care to uplift their spirits and gently draw out sensitive information without hurting them.

Xinhui (back row) with her brother (middle) and sister (front row). Her brother passed away from colon cancer when she was 24 years old. She had been his main caregiver. Photo courtesy of Xinhui Ng.
Palliative treatment is multi-dimensional and systems-focused, addressing the physical, emotional and psychosocial health of the patient, taking into account family dynamics and circumstances.
“I was awed. It’s such a tough topic to talk about dying – it’s really a skill,” said Ng.
A reckoning
Ng had been her brother’s main caregiver in his final month as the effects of the cancer finally took its toll on him after two years of relatively good health.
“My dad already lost his wife. And he was going to lose his only son – it was very difficult.”
“It was very stressful to witness him being ill,” Ng said as she recalled her turmoil and helplessness as she looked after her brother. She was still a young nurse with only a few years of experience. As his condition worsened, Ng often found herself praying that God would take him home.
Keenly aware of the distress that her father was experiencing, Ng held her emotions at bay and did not allow herself to cry at home. Her mother had passed away from the same cancer when Ng was seven.
“My dad already lost his wife. And he was going to lose his only son to the same illness,” she said. “There was a lot of tension, it was very difficult.”
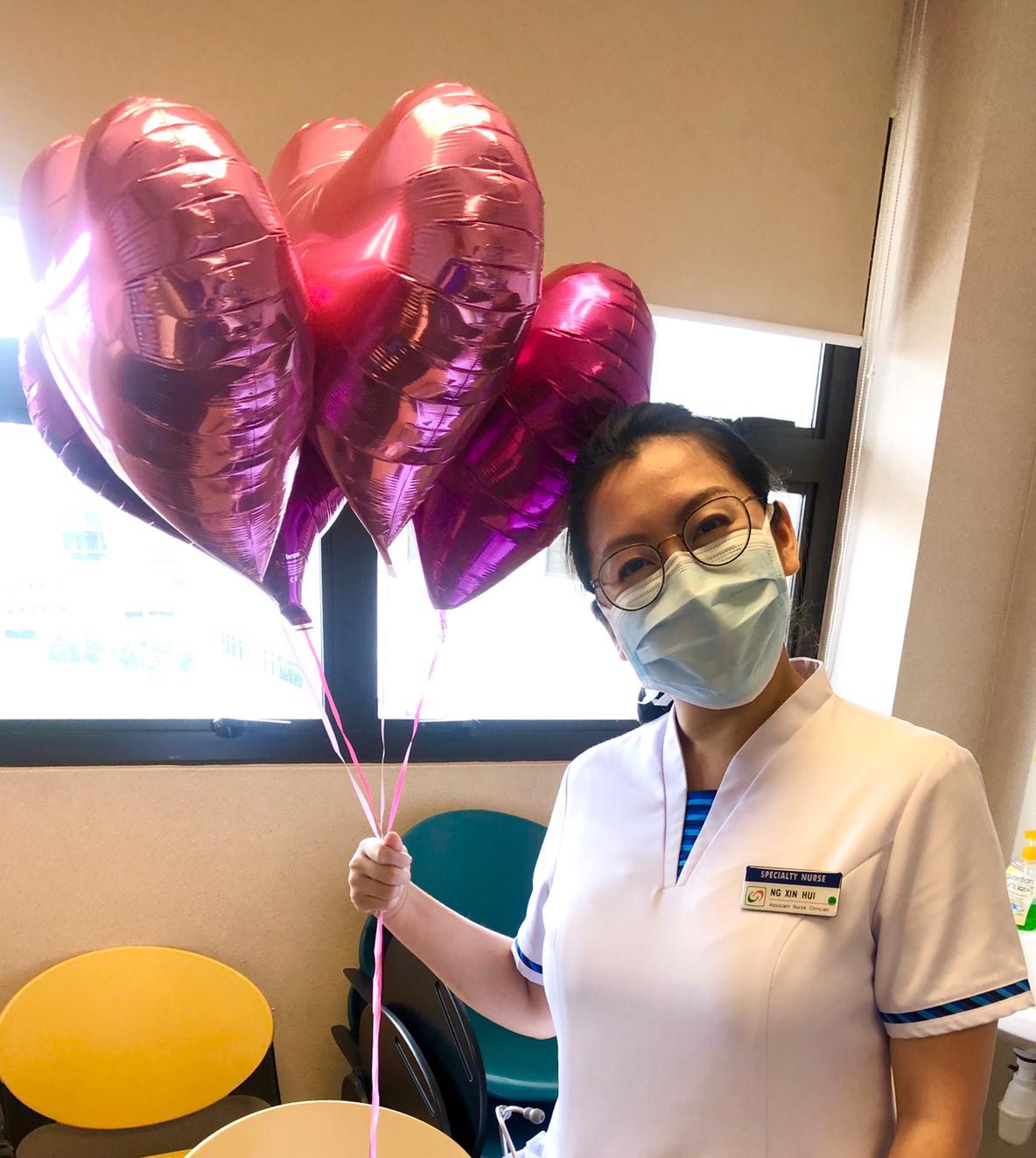
Xinhui joined the palliative care department in the National Cancer Centre of Singapore in January this year. Photo courtesy of Xinhui Ng.
At 33, as Ng reckoned with the pain of losing her brother and the brevity of life, she reconsidered her role as a nurse and her interest in palliative care.
So, after exploring various other nursing roles that included a stint at Assisi Hospice, Ng joined the palliative care department of the National Cancer Centre of Singapore (NCCS) in January this year.
A different aura
The distinctive characteristics of palliative care arise from its fundamental emphasis on the consideration of the patient as a multi-dimensional being. More than 20 years earlier, Sister Eliada Yap, a ward nurse in Tan Tock Seng Hospital’s surgical ward had been drawn to these very characteristics.
“They were like angels walking into the ward – their presence was so calming!”
“I noticed that they had a very different approach,” she said, referring to Professor Pang Weng Sun and Dr Angel Lee, who were early practitioners in palliative care medicine in Singapore. “They were like angels walking into the ward – their presence was so calming!”
In the surgical unit, the emphasis was on the surgery and a quick recovery. When patients were deemed no longer curable, they would be referred to either of the two doctors who were part of the geriatrics department at that time. (Geriatrics was still relatively new and end-of-life care was considered a part of the specialty because of the association between death and the elderly.)
Professor Pang and Dr Lee would come in, take a chair and sit beside the patient to talk – sometimes, they even held patients’ hands. “I never saw the surgeons do that,” Yap exclaimed.
“When the patients see them, they are at ease and share freely … I was very inspired!”
Yap decided to learn from them so that she could serve her patients better. At 18, Yap became a Christian and decided from then on that she did not want to become an accountant because she wanted a more “caring” profession.

Sister Eliada Yap (extreme left) with the first hospital-based palliative care service team in Tan Tock Seng Hospital in 1998. It was a multi-disciplinary team consisting of doctors, therapists, medical social workers and nurses, including Dr Angel Lee (middle, front row). Photo courtesy of Eliada Yap/Assisi Hospice.
“My direction in life changed. I didn’t want to just sit there and look at numbers,” said Yap, who became a nurse in 1988.
Almost a decade later, she was invited to join Professor Pang and Dr Lee in their newly-formed team which was the first hospital-based palliative care service in Singapore.
Continuity of care
The field of palliative care in Singapore has grown significantly in the last two decades with various hospices and organisations set up, either independently or within hospitals. Centred on the idea of a “good death”, palliative medicine takes a multi-disciplinary approach – involving doctors, nurses, social workers and even others like music and art therapists.
A patient’s dignity is of priority, and care is taken to surround him or her with the warmth of human contact through loved ones and familiar faces. Helping the patient leave this world in peace, with no unfinished business, is the gold standard.
“To me, patients need not suffer when they are dying,” said Yap.

Sister Eliada Yap pursued further studies in palliative care, earning her Masters while in Melbourne, Australia. She worked there for several years before returning to Singapore. Photo courtesy of Eliada Yap/Assisi Hospice.
Yap, who has since completed her Masters degree in palliative studies and is now the senior nurse manager at Assisi Hospice, still remembers one of her early patients. Until today, his case remains a graphic reminder of the importance of a holistic, systems-based approach.
“He was a chicken wholesale seller who had cancer of the lung. His wife was visually impaired. They had four children – his eldest had special needs,” Yap said.
Having exhausted his treatment options, he was discharged to pass his last days at home. Arrangements were made and a helper was hired to help the family.
“I still remember that when I walked into his house, I saw all these green patches on the floor.”
But on the second day of caregiver training, the helper arrived crying: The house was so dirty that she did not know where to start cleaning. So Yap and a medical social worker rallied two volunteers – including Yap’s husband – to make a home visit. “We needed to support his helper and make it easier for her. We didn’t want her to run away.”
Sparing no details, Yap described the scene that they saw when they arrived. “I still remember that when I walked into his house, I saw all these green patches on the floor. They looked mouldy and I was wondering what it was.
“I realised that – my gosh – it’s actually the sputum of the patient.”
The phlegm he’d spit out between coughing fits had not been cleaned up – his wife’s severe visual impairment meant that she could not see the patches.
“Right there, I tell you, I wondered if this is what it would take for me to prepare a patient to go home,” Yap said honestly, as she shared about the thick grime that covered the walls of the kitchen and toilet and the discoveries of black insects in plastic bags of dirt.
After nine months, the patient passed away. “But he had good times with his wife and that was very good closure for all of us,” Yap shared. “I learnt a lot from this about the resources needed from community and how to ensure a continuity of care from hospital to home.”
Not just a waiting game
Well-meaning friends had cautioned Ng about the emotional toll that came with the job.

Xinhui (left) might still be relatively inexperienced in palliative care, however, she knows that even though the journey ahead will not be easy, God has shown Himself faithful. “Good or bad or tough, God brought me to it, so He will bring me through it.” Photo courtesy of Xinhui Ng.
But during her time as a ward nurse, Ng says has seen “too many” patients who have passed on that she wishes could have been referred for palliative care earlier. When doctors say treatment options are “limited”, it is not the end of the world.
“If we are able to help them – achieve certain goals or allay the anxiety of their caregivers, these are positives. We are there to journey with them.”
It is not about “waiting to die”, she pointed out. “Life is very, very short – and I don’t say that lightly. Since all of us will die one day, we should focus on what we can do to have a better quality of life in the time that we have.”
“In situations like this, it is the Holy Spirit who prompts me. If not, sometimes, it is too overwhelming.”
However, the reality of death, pain and symptom-induced suffering that patients face often mean that they often look for some spiritual support and there are common questions that arise like, “Why me?”
“I cannot answer that,” said Yap. “But they already have the answers, and it is just a matter of how to approach it and draw out the concerns or issues they have.”
Addressing patients’ psychosocial needs is a skill that Ng is still working on: “Each person reacts differently so you have to convey the message to them in individual ways.
It is important to listen and to facilitate this talk because there is “a lot” that can be done to help them. “But I can never be over-prepared for such discussions,” she said, adding that she always prays before each conversation because sometimes there are situations that“go beyond our imagination”.
“When I walk into situations like this, it is God who is guiding me. The Holy Spirit prompts me – if not sometimes, it is just too overwhelming. I have to be very sensitive to His leading so that I can help the person at that moment.”
In Him and through Him
That guidance also extends to Ng’s circuitous route into the field of palliative care.
“God has His ways to lead,” said Ng. “There was a period I feared that God would take someone away from me again, but down the road, I think the message from God was more that He just wants us to depend on Him, and to do so wholly.
“Good or bad or tough, God brought me to it, so He will bring me through it.”
It is a “simple” faith that Yap holds to. After each patient passes on, Yap gives herself space to find closure with her husband, her team or even her mentors.
There is one particular emotion that has kept her in this field for over 22 years.
“Joy is an important part of my role,” Yap said. “Without it, it would be difficult to bring hope to my patients and my team of caregivers.”
But she recognises that God holds her centre and it is His joy that she receives each day. “God is my strength. Without Him, I cannot do this for the long haul,” she said.
This is the second story in a series of interviews to commemorate Singapore Nurses’ Day on August 1, 2020. You can find the other stories are below.
On the frontlines and far from home: Two foreign nurses draw comfort from giving comfort
“Less of me and more of You”: A nurse’s journey from aesthetic medicine to end-of-life care
We are an independent, non-profit organisation that relies on the generosity of our readers, such as yourself, to continue serving the kingdom. Every dollar donated goes directly back into our editorial coverage.
Would you consider partnering with us in our kingdom work by supporting us financially, either as a one-off donation, or a recurring pledge?
Support Salt&Light



