Loving “care-frontation”: 8 answers for lay people on helping those with mental health needs
by Gemma Koh // July 18, 2022, 8:56 pm

The Covid-19 pandemic has triggered a 25% increase in the prevalence of anxiety and depression worldwide. How do lay counsellors and mental health professionals work together to help those in our midst? Photo by Hanna Morris on Unsplash.
“Even if Covid-19 settles down, experts are saying that its consequences – especially in terms of mental health problems – will last for seven to 10 years afterwards.”
The Covid-19 pandemic has triggered a 25% increase in the prevalence of anxiety and depression worldwide.
So said Rev Dr Tan Siang Yang, who was in Singapore, speaking on the first night (July 7) of the Christian Mental Health Conference (CMHC) 2022.
“The Covid-19 pandemic has triggered a 25% increase in the prevalence of anxiety and depression worldwide. This is a wakeup call – according to the World Health Organisation – to all countries all over the world to step up mental health services and support,” said Rev Dr Tan, in his talk Helping People in Need, Being a People-helper.
Rev Dr Tan, a retired senior pastor, is also the senior professor in psychology at the Graduate School of Psychology at Fuller Theological Seminary in Pasadena, California.
There are not enough professionals in the world to meet the substantial increase in mental disorders, even with the push towards digital means of therapy and counselling, he said.
“The church has to play a central and crucial role because God has called us to care for one another.”
In the last year, there has been a call for more lay counsellors to meet this tremendous need.
“The call for lay counselling comes from professionals in the field – not by Christians, not by churches,” he added.
Where does the Church come in?
“The Church has to play a central and crucial role because God has called us to love our neighbours as ourselves, to care for one another, to carry each other’s burdens,” said Rev Dr Tan, who also spoke about the biblical basis for counselling (read about it here).
The talk drew an abundance of questions from the 800 viewers over live-stream and an audience of 200 who were present at the conference held in Bethesda (Bedok Tampines) Church (BBTC).
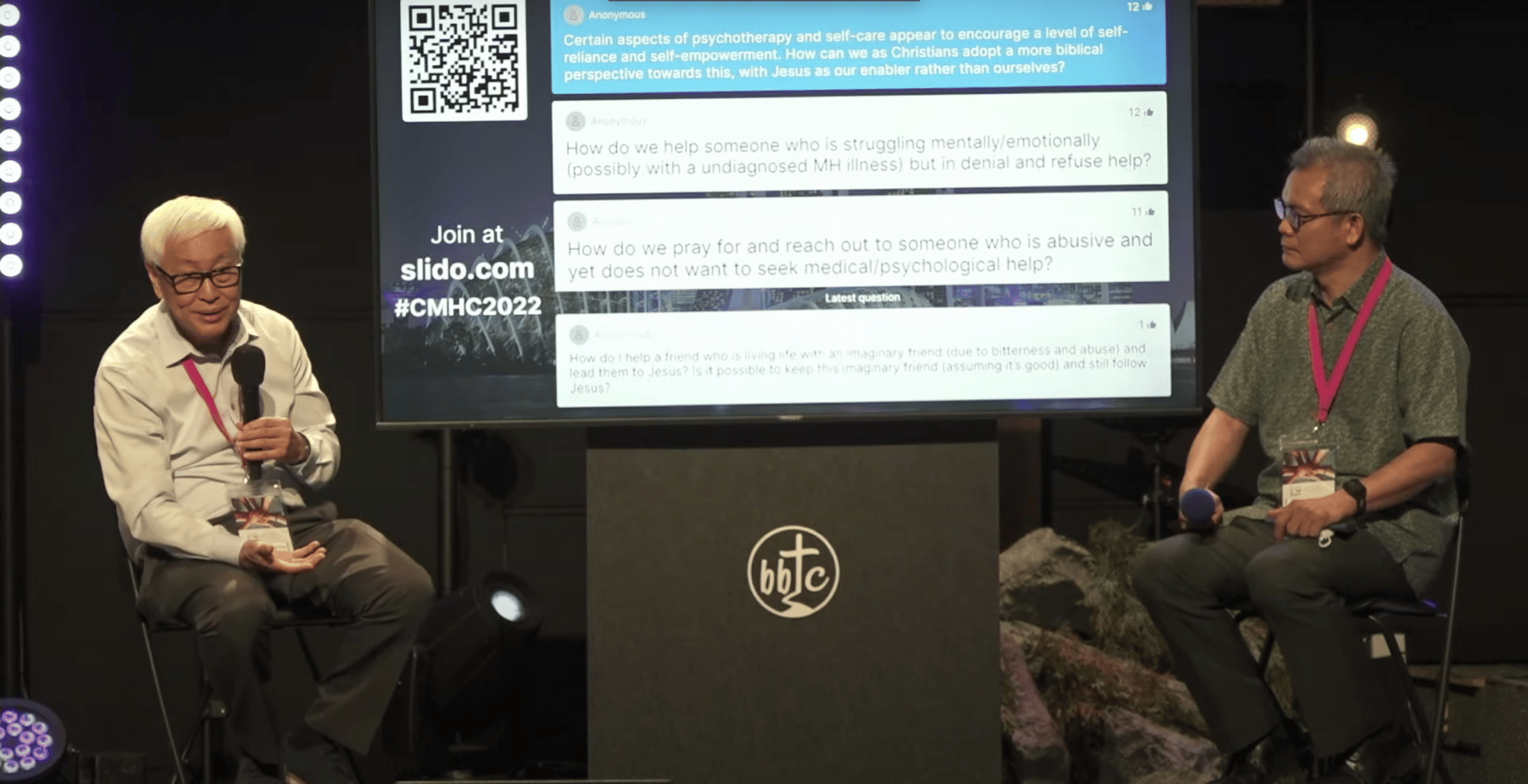
Rev Dr Tan Siang Yang (left) with Ps Chua Seng Lee at the Christian Mental Health Conference 2022.
Rev Dr Tan addressed the questions (below) that received the most votes via Slido.
Rev Dr Tan is well-placed to speak from both roles as pastor and psychologist, said Ps Chua Seng Lee, who hosted the session. “He understands the tensions of a pastor and he understands the science behind psychology.”
Ps Chua is co-chair of the CMHC, and Deputy Senior Pastor of BBTC.
(The following Q&A has been edited for clarity and brevity).
1. What is the role of mental health professionals in supporting the mental health needs of the Church?
Rev Dr Tan: We should refer the most severe cases to mental health professionals. They should also support pastors, and they should also be involved in training lay counsellors, giving seminars and conducting workshops for the church and so on. It must not be one sided.
So that’s why this conference is so important: We are all networking. We work hand in hand.
Ps Chua: Many professionals are the best-kept secret the church; the church pastor doesn’t know they exist.
So it’s important for you to come out from hiding to identify yourself so that your pastor knows how to get you involved in this matter of work.
2. How can church leaders support Christians who may be on the verge of suicide and self-harm? Where do we draw the line?
That’s a tough one.
We no longer say someone “committed suicide”. That suggests “you committed a crime”. Suicide is not a crime. It is a very painful thing. When people take their own life, they are not in the state of mind to think straight. They are often deeply depressed, they are not rational.
When somebody comes to you and says: “I’m feeling so bad, I have no hope anymore. I’m going to kill myself. I want to end it all”, don’t just say, “Eh, you’re pulling my leg, ah?”
You’ll have to ask some questions – questions that lay people often dare not ask because they think if they ask those questions, you’ll make people engage in suicidal acts. No (that is not true).
“When people take their own life, they are often deeply depressed, they are not rational.”
Ask: “Tell me more. You say you want to take your own life. How often do you think about this? How intense it is?”
If the person says: “I think about it every day, 10 times a day. And when I think of it, I almost do it”, that is serious.
Then ask the most important question: “What plan do you have?”
If they say: “Oh, I have a bottle of 100 sleeping pills” or “I’m going to jump down from the flat”, you cannot take that lightly.
Immediately, as much as you can, take them to the emergency department of a hospital, get them assessed by a psychiatrist there. They may need to be hospitalised. That is the best favour you can do for them to save their lives.
If they refuse, you will have to alert certain people. You may have to call the police if it’s an emergency.
We need to take suicidal intentions seriously, because if we don’t, that person might take their own life the next day and it’ll be too late.
3. What are your thoughts on mindfulness based therapy?
Rev Dr Tan: The latest development in the field of cognitive behaviour therapy (CBT is Rev Dr Tan’s area of expertise) is mindfulness based therapy. It has at least four major approaches; all have common elements:
1. Acceptance: Let the thoughts come, let them go, don’t fight them.
2. Mindfulness: Paying attention to the here and now and your breath, for example.
They are not necessarily based on eastern mystical approaches, though some are. Most don’t involve blanking out your mind.
The main emphasis is on concentrating on your breath.
You are slowing down and focusing on the present, with no judgement, with no censure. You are not stuck in the past, you are not worrying about the future.
“In Christian mindfulness, you’re not just concentrating on your breath. You’re concentrating on the Lord.”
Overall, research shows that the mindfulness approaches are quite effective. They help people slow down, they help overcome anxiety, depression and stress. So it’s not a bad thing, except it depends on the version of mindfulness.
In Christian mindfulness, you’re not just concentrating on your breath. You’re concentrating on the Lord (“Lord have mercy”); on a verse (“Be still”, Psalm 46); or peace from Christ (“Jesus my peace”), or the Jesus Prayer based on Luke 18. (“Lord be merciful to me, the sinner.”), for example. And repeating these phrases.
Try that sometimes when you cannot pray. Sometimes if you can’t even say 12 words or five words, just say: “Jesus help me.”
Jesus did not speak against repetition. Jesus spoke against vain repetition.
Mindfulness is not a bad word. Don’t throw the baby out with the bathwater.
Three authors have written books on Christian mindfulness: Joshua Knabb, Regina Trammel and Dr Fernando Garzon.
4. When should we step in to help a depressed individual who is passive?
Rev Dr Tan: When people are really depressed, don’t tell them: “Just snap out of it.” It’s not so easy. If it was so easy, they would snap out of it.
In major depression and also in schizophrenia, suicidal risk is the highest. You have to be careful. You listen, you support. But it’s true – you must not reinforce too much passive behaviour.
So you can tell the person, for example: “I can understand now that you’ve told me more. This must be very hard for you. Are you seeing someone for some medication?”
If they say: “Yes, I’m taking the anti-depressants”, ask “How long has it been?”
Then: “How do you feel?”
They may say: “As bad. If not worse”.
There are often side effects, such as dry mouth and sweaty palms.
Antidepressants take anywhere between three to seven weeks to work. But be careful when anti-depressants kick in, and the depressed patient suddenly feels very good but still not good enough. Their energy has suddenly gone up. That’s the highest risk for suicide because they have enough energy to do it. Before that, they’re so down, they are thinking about it but have no energy to do it.
“Our guard comes down because we think they have recovered when say they feel better after taking medication.”
Ps Chua: As caregivers, our guard comes down because we think they have recovered when say they feel better after taking medication. We need to continue to monitor them.
Rev Dr Tan: Some of the anti-depressants have the side effects of increasing suicidal ideation in Week One or Two, and they feel even more suicidal. So it is important to keep in touch with the person you are helping and tell them to call their psychiatrist if they feel worse.
A good psychiatrist will change the medication or dose. If you are not a psychiatrist, don’t tell them to change the dose or medication – that would be malpractice.
Suggest baby steps to help them overcome their passivity. Don’t suggest something that takes enormous amounts of energy to do because you’re going to set them up for failure and they’ll feel worse.
I encourage all my patients who have depression or anxiety to exercise … small baby steps at a time. Don’t ask them to run three miles. Encourage them, slowly but surely, to walk everyday – just three yards or one block. Walking is one the best exercises.
“Suggest baby steps to help them overcome their passivity.”
Encourage them also to eat properly and practise good nutrition.
The latest research shows is that your gut health affects your brain health which affects your mental health. So probiotics are important.
If you don’t want to spend 50 bucks for a bottle of probiotic pills, eat more kimchi, yoghurt or pickled stuff. They all contain probiotics.
Supplements like fish oil or Omega three fatty acids can also help.
There is such a thing called “loving care-frontation” (coined by author David Augsburger) of depressed people. Do it in a gentle and caring way, bit by bit.
5. Certain aspects of self-care appear to encourage a level of self-empowerment. How can Christians adopt a more biblical approach?
Rev Dr Tan: The biblical perspective eventually is self-denial, surrender to Jesus – not self-effort or self-improvement.
So the first step of therapy is to help them to come to accept themselves more and to empower them to take baby steps to improve self-confidence. At the same time, if they are Christians, I pray with them to take the next step of surrender to Jesus. So you can combine the two right from the start.
“Counselling is not the same as evangelism. But there is a place for gently sharing the Gospel.”
But what if you’re counselling a non-Christian? They don’t believe in Jesus. You cannot bring Jesus into the picture. You cannot disciple them. You still counsel them; you are still compassionate and loving enough to help them feel a bit better.
When I’ve helped a non-Christian feel better, sometimes they say: “Thank you, Dr Tan, for helping me. You are the most loving doctor. So what’s your secret?”
Then I would say: “You really want to know? It’s Jesus.” If they give me permission, I will tell them about Jesus. Usually, I would refer them to a church to a pastor.
You have to be careful of the dual role and power differential. You’re not there to convert people.
Counselling is not the same as evangelism. But there is a place for gently sharing the Gospel.
6. How do you help someone who is struggling mentally or emotionally, but is in denial?
Rev Dr Tan: If they are dangerous or at suicidal risk, you can bring them to the emergency section of the hospital, even if they don’t want help.
But if they are troubled or emotionally unstable, but still have their rational mind, you cannot force them to get help, especially if they have their faculties intact.
Sometimes you just have to wait until they’re willing to get help. But meanwhile, don’t give up. You either have to encourage them or persuade them to get help. Or talk to their parents. Or if you have the permission, see whether other people can convince them (to get help).
“The Church must be equipped. So when the person appears in our lives, we can proactively reach out to the person.”
If they get worse, they might be desperate. That’s why there’s an approach to therapy called motivational interviewing (MI is developed by William Miller and Stephen Rollnick).
They spend a lot of time in the first two sessions empathising with their clients, saying things such as: “So this must be very hard for you, you have a lot of ambivalence whether you want to change or not. In fact, you really don’t even know whether you want to seek help.”
You empathise with them, you give them a lot of support. And when they trust you and feel you understand them, they might say: “Maybe I can try one step.” Then you can do more. So you have to be very patient.
I would also say, pray for the client, that the Holy Spirit will somehow touch them.
Ps Chua: Having mental health issues is a double whammy; the person is in need, and may not have the willpower to seek help.
That’s why the Church must be equipped to have this conversation. So when the person appears in our lives, we can proactively reach out to the person and practise the skills we’ve learnt. I want to encourage you (viewers) to get trained.
Rev Dr Tan: You can learn some important basic skills for lay counselling in a weekend or sometimes in two to three months if you have the time.
You are learning to listen, to come alongside someone, to ask good questions. Those things can be taught in a short period of time. (See below for a organisations that can equip you.)
It would be very helpful for the church to organise say an adult class, or a four-week module or seminar on learning listening skills.
7. At which point should we refer the person to seek medical treatment, rather than relying solely on prayer and dealing spiritual roots?
Rev Dr Tan: It’s okay to start with spiritual and biblical counselling and prayer. But after about three weeks, if the person is not getting better but worse, or the depression is getting worse and suicidal ideation increasing, you need to refer them to seek medical treatment.
It’s wise to say: “I sense something beyond me. It’s not just a psychological or emotional thing. It may be a biologically-based depression.”
When you refer, don’t put down the client. Don’t say: “You are beyond redemption, I cannot help you.”
Instead say: “I’m just a lay counsellor/pastor” or “I don’t have enough experience or expertise in this area, but I know someone who specialises in this. I think he can help you more. But I’ll continue to follow up with you, and pray with you.”
Don’t abandon them.
There is training where you can learn when to refer, how to refer, who to refer to. All these are skills.
Whenever someone comes to see me in private practice, after four to five weeks, they usually get better. But if they get worse, I’ll refer them to a psychiatrist or a medical doctor to get some medication.
I’ll explain to them rationally: “You need better help than I can give. I’m not a medical doctor, so I cannot prescribe. Try it together with counselling – it will be more effective.”
8. How do you help someone with Narcissistic Personality Disorder?
Rev Dr Tan: If you are a lay counsellor, don’t diagnose.
The best thing you can do is to refer them to a professional.
Narcissistic Personality Disorder (NPD) is a difficult diagnosis to make. It doesn’t mean the person is selfish. We are all narcissistic to a certain extent; narcissism, selfishness, self-centredness is a major characteristic of the sinful nature of man.
“You may not know their background, how much they suffered as a kid, but you’ll become more patient with them.”
But Narcissistic Personality Disorder is much more severe. If the person is very self-centred, cannot think of other people, they might need help. But the real narcissist is the last person to seek help because he thinks he’s god’s gift to humankind. “You need my help. I don’t need your help,” he might say. Don’t try to argue with him.
A person with NPD is not just someone who is not other-centred. This person may have suffered tremendous injury to their sense of self when they were growing up. Because of harsh parents, authoritarian parenting, abuse, neglect, for example, they became narcissistic – not because they are so selfish, but because they are so broken.
Once you understand that, you become more empathic toward them, rather than just thinking: “This guy the most selfish person I know”.
You may not know their background, how much they suffered as a kid, but you’ll become more patient with them.
That’s why therapists who are good with NPD are very patient. Is it easy to help them? No. As with other personality disorders, they are very difficult to help.
Watch Helping People in Need, Being a People-helper on YouTube here.
Some of the material from the talk is from Rev Dr Tan Siang Yang’s books: Lay Counseling: Equipping Christians for Helping Ministry (revised and updated in 2016); Shepherding God’s People: A Guide to Faithful and Fruitful Pastoral Ministry; and Counselling and Therapy: A Christian Perspective.
Where you can get equipped
The Association of Christian Counsellors is in the midst of setting up a lay counselling training framework. They are looking at partnering with pastors and churches to help them develop training programmes for lay counsellors. Interested pastors and churches can register interest here by July 31, 2022.
The following secular organisations offer equipping in basic skills to individuals and groups:
- Character and Leadership Academy: Its QPR Gatekeeper workshops teach inter-religious organisations (including churches) and secular groups suicide prevention skills. The three-step QPL method stands for question, persuade, refer. Ps Chua Seng Lee is its founding chairman of CLA. Contact them via Facebook or via their website: characterleadership.sg
- Caregivers Alliance: Training programmes for caregivers help attendees understand different mental health issues including depression, anxiety disorder, psychosis, schizophrenia and dementia. They aim to increase communication and problem solving skills and teach coping strategies. They also give workshops on trauma informed care. Website: cal.org.sg
- Caring for Life: LIFE Training is a half-day (four-hour) training programme that equips participants to engage persons who might be having thoughts of suicide, and connect them with community resources for suicide intervention. Website: caringforlifesg.org
- Samaritans of Singapore: SOS offers a range of training programmes and workshops for the public. They also offer in-house training (regular workshops or customised programmes) for organisations. Topics include responding to someone who may be suicidal, active listening, and empowering the elderly and their caretakers to seek help. Website: sos.org.sg
RELATED STORIES:
Journeying with the depressed and suicidal: Tips for “people helpers”
“Suffering can draw us back into the life that God intended for us”: Tips for people helpers
We are an independent, non-profit organisation that relies on the generosity of our readers, such as yourself, to continue serving the kingdom. Every dollar donated goes directly back into our editorial coverage.
Would you consider partnering with us in our kingdom work by supporting us financially, either as a one-off donation, or a recurring pledge?
Support Salt&Light